Key Takeaways
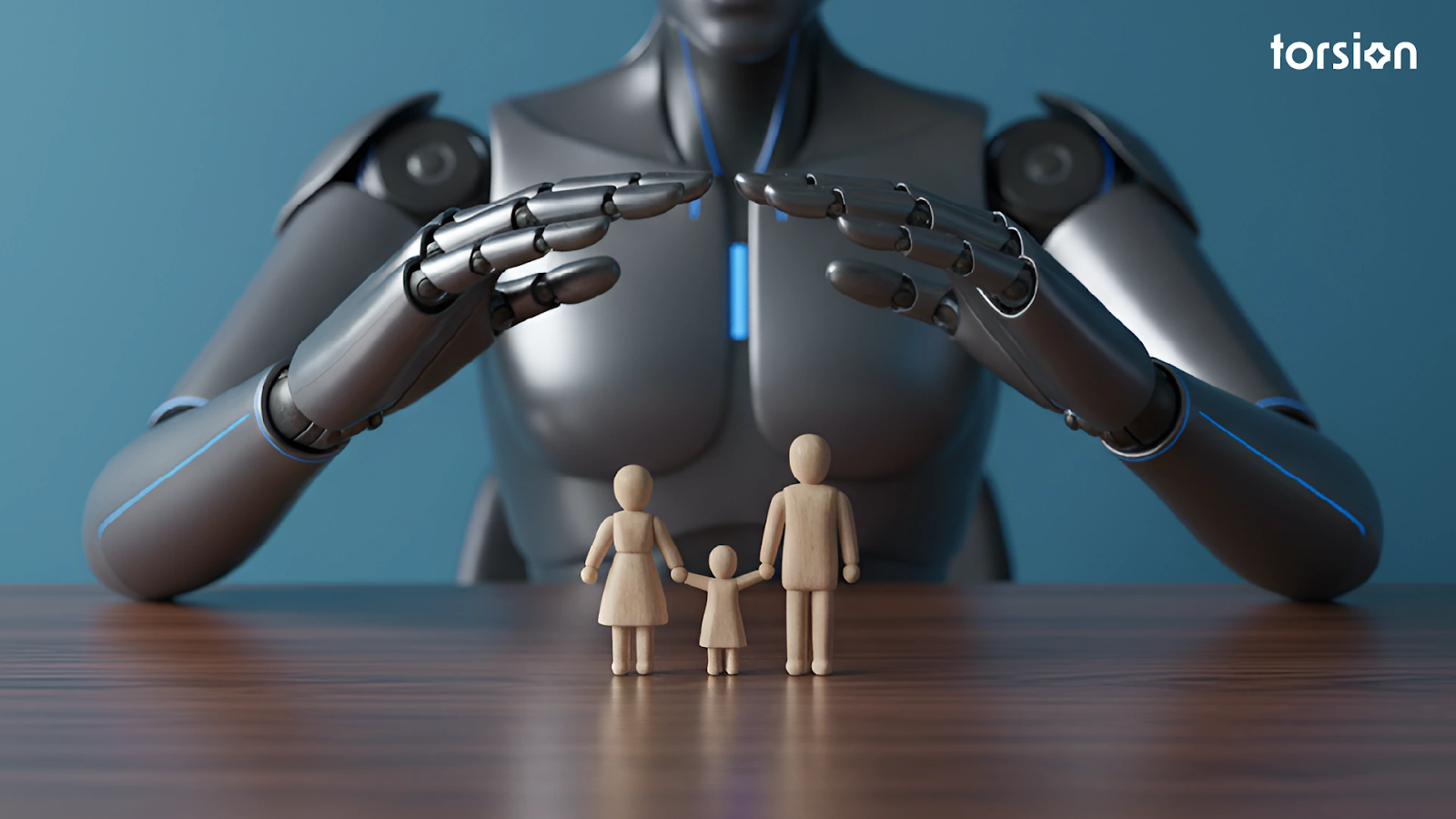
- Massive Untapped Value: Healthcare payers have an opportunity to unlock a staggering $200 billion in value, yet 97% of their data currently goes unused due to fragmented, legacy systems.
- Urgent Financial Pressure: With medical loss ratios hitting 90-92% and administrative tasks consuming up to a third of all healthcare spending, operational efficiency is a survival imperative.
- Proven ROI with AI: Leading health plans are already achieving significant returns through targeted AI automation, including saving $25 million in operational costs and reducing administrative overhead by up to 30%.
- Beyond “Pilot Purgatory”: While 74% of payers are increasing IT spending, the key to success lies in moving beyond isolated pilot programs to a strategic, enterprise-wide AI implementation.
- Strategic Imperative: The transformation journey is complex, involving not just technology but also data governance, change management, and regulatory navigation. A clear blueprint is essential for success.
Your organization is likely spending more on IT and data infrastructure than ever before. In fact, 74% of healthcare payers have ramped up their technology budgets, pouring resources into modernization.
Yet, the core metrics are failing to improve and getting worse. Medical loss ratios are climbing to a staggering 90-92%, and administrative tasks still devour up to a third of all healthcare spending.
This creates a paradox that should keep every data scientist, engineer, and CTO in the payer space awake at night: Why is record-high investment yielding diminishing returns?
The answer isn’t in the technology itself. It lies within a stunning statistic: while a potential $200 billion in value is sitting within your systems, a full 97% of your data remains completely untapped.
This is the missed opportunity. The root cause behind the “pilot purgatory” that traps promising AI projects and the manual processes that keep claims in limbo for over a month.
What do the few payers who are breaking this cycle know that others don’t? It isn’t about having a bigger budget or a larger data lake. It’s about understanding a fundamental flaw in how most payers approach the relationship between their data, their legacy systems, and their AI strategy.
They are trying to solve a new-world problem with old-world thinking.
This guide is designed to expose that flaw and provide the blueprint to fix it. We will decode the paradox and reveal the specific strategies that separate the payers who are just spending money from those who are generating transformative ROI.
We’ll show you how to stop excavating pebbles and start mining the gold.
The Current State: Why Healthcare Payers Are Stuck in Digital Quicksand
The paradox of rising IT spend and worsening financial outcomes is the inevitable result of a foundational crisis. Industries like banking have successfully boosted digital channel usage by 30% and achieved an 8.2% total shareholder return from their tech investments.
But most healthcare payers remain trapped in a state of digital stagnation. They are caught in a cycle of “pilot purgatory,” where innovation dies before it can scale.
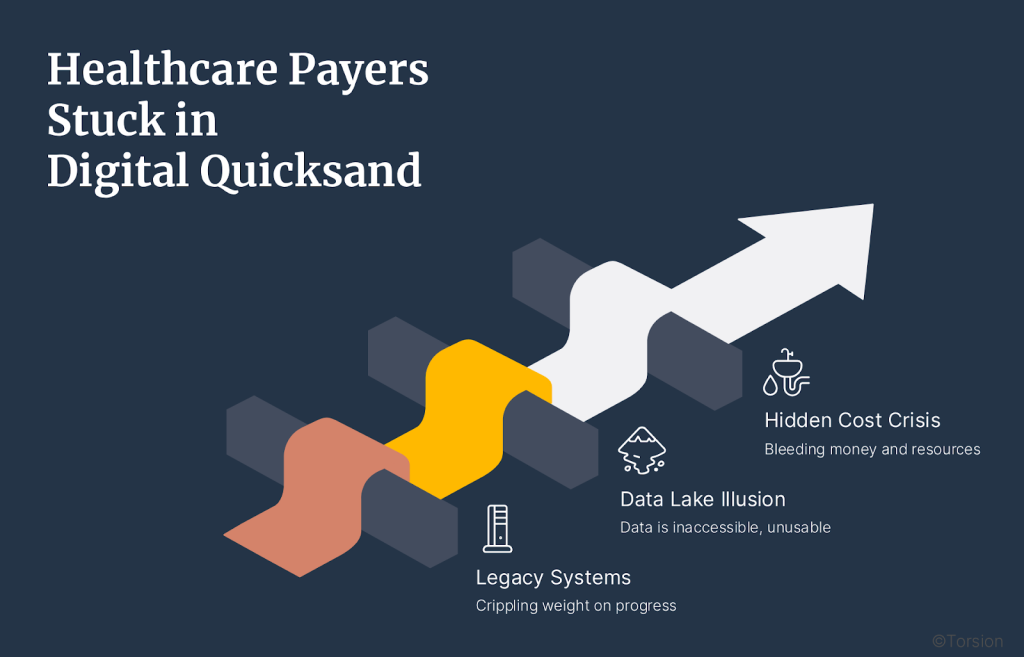
This isn’t due to a lack of effort. It stems from three deep-seated, interconnected problems that create a kind of digital quicksand: the more you struggle with isolated solutions, the deeper you sink.
1. The Crippling Weight of Legacy Systems
The core of the problem lies in the very infrastructure that payers rely on. An estimated 65% of payers report that their transformation efforts are severely limited by outdated and inflexible legacy systems. These platforms, often decades old, were never designed for the demands of real-time data processing or AI-driven analytics.
Instead of enabling innovation, they actively resist it. Payers are spending a colossal $15 billion annually just on maintaining these archaic systems.
Every dollar spent propping up a legacy core is a dollar not spent on developing competitive advantages. This environment creates a nightmare for data engineers, who must build brittle, complex bridges between old and new systems, slowing down projects and making true integration nearly impossible.
2. The Illusion of the Data Lake
For years, the prevailing wisdom was to build a massive data lake. The thinking was, “If we just get all our data in one place, value will follow.” The reality has proven far more complex. While payers have amassed vast oceans of data, they’ve created a new problem: a data swamp.
A staggering 97% of healthcare data goes unused because it is fragmented, unstructured, and lacks the governance needed to be actionable. Without a robust data strategy that includes ingestion, cleansing, normalization, and semantic consistency, a data lake is just a storage expense.
Data scientists spend up to 80% of their time just cleaning and preparing data instead of building models that drive value. Your organization may have the data, but it lacks the connective tissue to make it intelligent.
3. The Hidden Cost Crisis Bleeding You Dry
While IT teams focus on grand modernization projects, a silent financial crisis is unfolding in the operational departments.
- Administrative Bloat: Manual processes for claims, prior authorizations, and member services are not just inefficient; they are cripplingly expensive. In some cases, administrative tasks account for 40% of total hospital costs, a burden that ultimately gets passed back to payers.
- Fraud and Waste: The industry loses an estimated $300 billion annually to fraud, waste, and abuse. Without sophisticated AI monitoring, payers are attempting to plug these massive leaks with manual audits, which is like trying to catch a river in a bucket.
- Regulatory Drag: Only 11% of payers feel prepared for emerging GenAI regulations. The fear of non-compliance causes many to default to slow, manual processes, creating a drag on the entire organization and leaving them vulnerable to more agile, tech-forward competitors.
This is the digital quicksand: a foundation of legacy tech, a swamp of unusable data, and a relentless financial bleed from operational inefficiency. Pouring more money into this broken foundation won’t fix the problem.
The only way out is to fundamentally rethink the blueprint for transformation.
The AI Transformation Blueprint: From Quicksand to Solid Ground
Escaping the digital quicksand doesn’t happen by chance or by funding yet another isolated pilot project. It requires a deliberate, architectural approach: a blueprint that builds a solid foundation before attempting to construct a skyscraper. The goal is to move from a state of reactive spending to proactive, strategic execution.
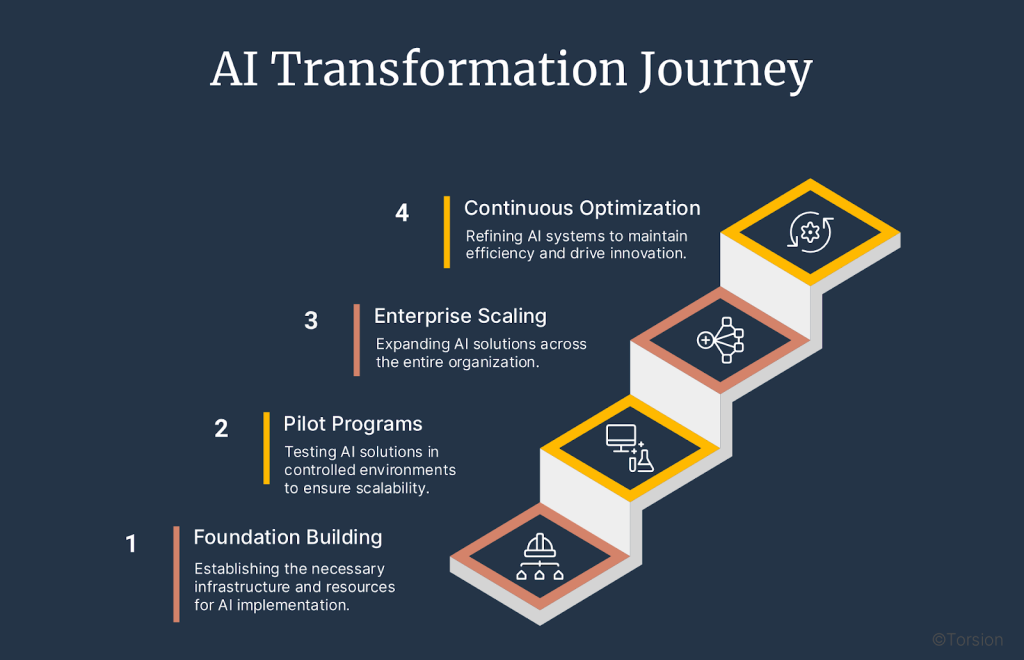
This transformation journey unfolds across four distinct but overlapping phases. This is not a rigid, one-size-fits-all plan, but a strategic framework that can be adapted to your organization’s unique maturity level and priorities.
Phase 1: Foundation Building (Months 1-6)
Before you can run a single AI model in production, you must have a foundation capable of supporting it. This initial phase is the least glamorous but the most critical. Rushing this step is why most transformations fail.
- Radical Data Governance: Move beyond simply storing data. The focus here is on creating intelligent data. This means establishing robust data ingestion pipelines, automated cleansing and normalization processes, and a semantic layer that ensures data is consistent and business-ready. This directly tackles the “data swamp” problem where 97% of data lies dormant.
- Strategic Modernization (Not Replacement): A full “rip and replace” of legacy systems is often too costly and disruptive ($15B annually industry-wide). The smart strategy is to wrap, not replace. Use modern APIs and abstraction layers to create a service-oriented architecture around your legacy core. This isolates the old systems while allowing new AI applications to interact with their data in a controlled, efficient manner.
- Proactive Compliance Frameworks: Don’t wait for regulators to dictate your AI strategy. With only 11% of payers feeling prepared for GenAI rules, building a proactive governance framework is a competitive advantage. This involves creating auditable, transparent AI models and establishing clear policies for data privacy, security, and ethical use from day one.
- Orchestrate Change Management: Technology is only half the battle. A staggering 64% of CEOs see employee adoption as a critical barrier. This phase involves securing executive buy-in, identifying departmental champions, and communicating a clear vision of how AI will augment, not replace, human expertise.
Phase 2: Pilot Programs with Scale in Mind (Months 4-9)
With a solid foundation, you can now launch pilot projects. The key difference here is that these pilots are not experiments; they are the first step of an enterprise-wide rollout. You must select use cases that are not only high-impact but also highly scalable.
- Target High-Impact, Low-Resistance Areas: Start with the most painful and least controversial problems.
- Claims Processing: Automating this function can reduce processing times by up to 85% and achieve near-perfect accuracy. This delivers immediate, measurable cost savings and frees up skilled adjusters to focus on complex cases.
- Fraud Detection: Deploying AI models to analyze claims in real-time can start recovering portions of the $300 billion lost annually to fraud and abuse.
- Claims Processing: Automating this function can reduce processing times by up to 85% and achieve near-perfect accuracy. This delivers immediate, measurable cost savings and frees up skilled adjusters to focus on complex cases.
- Measure Everything: Define the key performance indicators (KPIs) for success before you begin. Track metrics like processing time, cost per claim, error rates, and employee satisfaction. This data is crucial for building the business case for the next phase.
Phase 3: Enterprise Scaling (Months 7-18)
This is where your transformation delivers exponential value. Using the success and learnings from your scaled pilots, you begin integrating AI capabilities across the enterprise.
- Cross-Functional Deployment: Break down the silos between departments. The insights from claims data can inform underwriting models; member engagement data can refine network management strategies. This is where you begin to leverage the full power of an interconnected data ecosystem.
- Deploy Advanced & Predictive Analytics: Move from automating tasks to predicting outcomes. This includes developing risk stratification models to identify high-risk members before they become high-cost, or predictive analytics to optimize provider networks and care management pathways.
Phase 4: Continuous Optimization and Innovation (Ongoing)
Transformation is not a one-time project, it’s a new operational state. This final phase is about creating a culture of continuous improvement fueled by AI and data.
- Establish a Center of Excellence (CoE): Create a centralized team of data scientists, engineers, and business leaders responsible for identifying new AI opportunities, maintaining governance standards, and disseminating best practices throughout the organization.
- Monitor and Refine: AI models are not static. They must be continuously monitored for drift, bias, and performance degradation. Implement MLOps (Machine Learning Operations) practices to ensure your models remain accurate, fair, and effective over time.
- Drive Market Differentiation: With a mature AI capability, you can now focus on true innovation. This could mean developing hyper-personalized member wellness programs, creating new value-based care models with providers, or offering dynamic, data-driven insurance products that your competitors cannot replicate.
High-Impact Use Cases Delivering Immediate ROI
The true power of the AI transformation blueprint is realized when it’s applied to solve real-world problems. While the potential applications are vast, a few critical use cases stand out for their ability to deliver rapid and substantial returns.
These are not speculative, futuristic concepts; they are proven strategies that leading payers are using right now to turn their biggest cost centers into sources of efficiency and value.
1. The Claims Processing Revolution: From Weeks to Minutes
The traditional claims process is the poster child for healthcare inefficiency: a 30 to 45-day marathon of manual data entry, review, and adjudication that is both costly and prone to error.
- The Problem: This manual process is a major driver of administrative bloat. It requires large teams of adjusters to handle routine claims, leading to high labor costs and slow reimbursement cycles for providers, which strains network relationships.
- The AI Solution: By deploying AI-powered claims agents, payers can automate up to 85% of the entire claims lifecycle. These intelligent agents ingest claims data (structured and unstructured), validate it against payer policies and member benefits, flag exceptions for human review, and process clean claims straight through. All in minutes, not weeks.
- The ROI Reality: The results are transformative. One leading health plan that implemented this approach slashed its operational costs by 30%, saving $25 million. Automation at this scale not only delivers massive cost savings but also achieves 99.9% accuracy, reducing costly rework and appeals while enabling skilled human adjusters to focus on the most complex and high-value cases.
2. Fraud Detection and Prevention: Securing the $300 Billion Leak
The healthcare industry loses an astonishing $300 billion annually to fraud, waste, and abuse (FWA): a financial hemorrhage that directly impacts payer profitability. Traditional “pay and chase” models, which rely on manual audits after payments have already been made, are grossly insufficient.
- The Problem: Fraudulent actors are sophisticated, and legacy rule-based systems are too slow and simplistic to catch complex FWA schemes. By the time a fraudulent pattern is identified, the money is often long gone.
- The AI Solution: AI and machine learning models can analyze billions of data points across claims, providers, and members in real-time to identify anomalous patterns indicative of fraud before the claim is paid. These systems can flag everything from upcoding and unbundling to phantom billing and identity theft with a level of precision that is impossible for human teams alone.
- The ROI Reality: The impact is immediate. Regional Blue Plans have successfully used AI to recover $10 million in overpayments, while a German statutory health insurer (SHI) is achieving $30 million in annual savings through AI-powered FWA detection. This moves fraud detection from a reactive, loss-recovery effort to a proactive, cost-avoidance strategy.
3. Member Experience Transformation: From Transactional to Predictive
In an increasingly competitive market, member experience is a key differentiator. Yet, for many payers, member interaction is limited to confusing explanations of benefits or long call-center wait times. This transactional relationship is a missed opportunity for engagement and cost management.
- The Problem: A lack of personalization and proactive support leads to member churn, poor health outcomes, and increased costs down the line. For example, 86% of physicians report that prior authorization delays, a major point of friction, negatively impact patient outcomes.
- The AI Solution: AI enables payers to build a hyper-personalized and proactive engagement model. AI-powered chatbots can provide members with instant, 24/7 answers to their benefits questions. Predictive models can identify members at risk for specific health conditions and prompt personalized interventions or wellness recommendations. This turns the payer from a passive administrator into an active partner in the member’s health journey.
- The ROI Reality: While direct financial ROI can be harder to measure here, the strategic value is immense. Improved member satisfaction leads to higher retention rates and better scores on quality measures like HEDIS and Star ratings, which can directly impact revenue, especially for Medicare Advantage plans. Furthermore, proactive interventions can reduce the incidence of high-cost events, delivering significant long-term medical cost savings.
Overcoming Implementation Barriers: Navigating the Gauntlet
A blueprint is not a magic wand. The path from strategy to execution is riddled with technical, organizational, and regulatory hurdles that can stop even the most well-funded initiatives in their tracks.
Acknowledging these barriers is the first step to dismantling them.
Here’s how to navigate the gauntlet and ensure your transformation project doesn’t become another statistic in “pilot purgatory.”
Technical Challenges and Solutions
These are the hard-system problems that make data engineers and CTOs lose sleep.
The Challenge #1: Legacy System Entanglement
As we’ve seen, 65% of payers are hamstrung by legacy infrastructure. These monolithic systems are brittle, poorly documented, and create immense gravity that pulls down any attempt at modernization. A full replacement is often too risky and expensive.
The Solution: Wrap and Abstract. Instead of a high-risk “rip and replace,” the most effective strategy is to build an abstraction layer around your legacy core. By using modern APIs and microservices, you can create a standardized way for new AI applications to securely access legacy data without being coupled to the underlying complexity. This approach de-risks the transformation, allowing you to build new capabilities on a modern tech stack while methodically and safely retiring legacy functions over time.
The Challenge #2: Data Interoperability Chaos
Your data is your most valuable asset, but it’s worthless if it can’t communicate. The lack of data standardization and the persistence of data silos are why 97% of healthcare data sits idle.
The Solution: Embrace a Semantic Layer and FHIR. True interoperability requires more than just moving data; it requires creating a shared understanding of what that data means. Implementing a semantic layer creates a “Rosetta Stone” for your data, translating disparate codes and formats into a single, consistent business language. Adopting modern standards like HL7 FHIR (Fast Healthcare Interoperability Resources) further accelerates this by providing a standardized, API-first framework for exchanging health information, making integration faster and more reliable.
The Challenge #3: Security and Privacy in the AI Era
With 75% of executives worried about data privacy and the security risks of AI, this is a non-negotiable prerequisite. Deploying AI models without a robust security framework is not just irresponsible; it’s a potential extinction-level event for your brand.
The Solution: Adopt a Zero-Trust Architecture in a Modern Cloud Environment. Moving to a secure, HIPAA-compliant cloud platform is foundational. It provides the scalable infrastructure and advanced security tools needed for enterprise AI. Furthermore, implementing a “zero-trust” security model, which assumes no user or system is inherently trustworthy, ensures that every data access request is authenticated and authorized, dramatically reducing the risk of both internal and external breaches.
Organizational Change Management
The most sophisticated AI is useless if your people won’t use it. This is the “soft stuff” that is actually the hard stuff.
- The Challenge: Cultural Resistance and Workforce Fear. Change is threatening. When employees hear “automation,” they often hear “replacement.” According to, this fear and the resulting resistance to adoption are among the biggest barriers to success.
- The Solution: Champion Augmentation, Not Just Automation. Frame the AI initiative as a tool for augmentation. The goal is to automate the tedious, repetitive tasks (like processing clean claims) to free up your skilled workforce to focus on the high-value, complex problems that require human judgment (like managing complex patient cases or negotiating provider contracts). Establish an AI Center of Excellence (CoE) to provide training, evangelize successes, and give employees a clear path to upskilling, turning them from skeptics into champions.
Regulatory and Compliance Navigation
In healthcare, you can’t just “move fast and break things.”
- The Challenge: Navigating a Complex and Evolving Regulatory Landscape. With only 11% of payers feeling prepared for emerging regulations around generative AI, many are paralyzed by the fear of non-compliance. The ambiguity around rules for AI model transparency, bias, and auditability can stall projects indefinitely.
- The Solution: Build for Transparency and Auditability from Day One. Don’t treat compliance as an afterthought. Your AI systems must be designed from the ground up to be transparent and auditable. This means meticulously tracking data lineage, documenting model-building decisions, and implementing robust monitoring to detect and mitigate bias. By creating an explainable AI (XAI) framework, you not only satisfy regulatory requirements but also build trust with internal stakeholders and members, turning compliance from a burden into a source of competitive advantage.
The ROI Reality: Measuring Transformation Success
For any transformation to gain and maintain executive support, its success must be measured in the language of the business: Return on Investment. While the technical achievements of an AI implementation are significant, they are merely a means to an end.
The ultimate metrics of success are found on the balance sheet and in key performance indicators that drive market leadership.

A comprehensive ROI framework for AI transformation looks beyond simple cost savings and encompasses three distinct categories of value.
Financial Metrics: The Hard Numbers
This is the bottom-line impact that gets the immediate attention of your CEO and CFO. Based on extensive analysis, the financial opportunities are staggering.
- Administrative Cost Reduction: This is often the most immediate and tangible return. By automating core processes like claims and prior authorizations, payers can target a 13-25% reduction in administrative costs. For a payer with $10 billion in annual revenue, this translates to $150 million to $300 million in direct savings that can be reallocated to growth initiatives or passed on to members.
- Medical Cost Management: AI’s predictive capabilities unlock the next frontier of savings. By identifying at-risk members, optimizing care pathways, and reducing fraud, payers can significantly lower medical expenditures. The potential savings here range from $380 million to $970 million for a $10 billion payer, driven by fewer high-cost emergency events and more effective, proactive care.
- Revenue Enhancement: Transformation isn’t just about saving money; it’s also about making it. AI-driven insights can help payers design more competitive products, improve risk adjustment accuracy, and boost member retention. These efforts can lead to revenue increases of $260 million to $1.24 billion, turning the IT department from a cost center into a powerful engine for growth.
Operational KPIs: Measuring Efficiency and Quality
These metrics demonstrate how the transformation is improving the day-to-day functions of the business, leading to a more efficient, higher-quality operation.
- Processing Speed: Time is money, and AI delivers dramatic improvements. The goal is to shrink claims processing times from 30-45 days down to minutes, an efficiency gain of over 85%.
- Accuracy and Error Reduction: Automation drives quality. By achieving 99.9% accuracy in processes like claims adjudication, payers can drastically reduce the costs associated with rework, appeals, and manual corrections.
- Member and Provider Satisfaction: While harder to quantify, the satisfaction of your key stakeholders is a critical KPI. Track metrics like Net Promoter Score (NPS) for members and reduced administrative burden for providers. Happier members are less likely to churn, and satisfied providers are more likely to remain in-network.
- Employee Productivity: Measure the impact of augmentation. Track how much time skilled employees are freed up from repetitive tasks to focus on high-value strategic work. This demonstrates that you are elevating your workforce, not just cutting costs.
Strategic Value: Building a Moat for the Future
This category captures the long-term, competitive advantages that a successful AI transformation provides. While these benefits may not appear on a quarterly report, they are arguably the most valuable.
- Competitive Differentiation: In a commoditized market, the ability to offer hyper-personalized plans, proactive wellness interventions, and a seamless digital experience becomes a powerful competitive moat that digital-laggard competitors cannot easily cross.
- Market Agility: An AI-native organization can adapt to market shifts and new regulations far more quickly than one bogged down by legacy systems and manual processes. This agility is a critical asset in the dynamic healthcare landscape.
- Innovation Capability: By building a robust data and AI foundation, you create an “innovation platform” that enables the rapid development and deployment of new products, services, and business models, ensuring your organization’s relevance and leadership for years to come.
Implementation Roadmap: From Strategy to Execution
Knowing the what and why is crucial, but execution is what separates market leaders from laggards. A successful AI transformation is not a single, monolithic project but a series of well-orchestrated phases.
The roadmap provides a practical framework to guide your journey from initial assessment to enterprise-wide optimization, ensuring that each step builds momentum and delivers measurable value.
1. Assessment Phase: Know Thyself
Before you can chart a course, you must know your starting position. This phase is about conducting a brutally honest evaluation of your organization’s current state.
- Conduct a Readiness Assessment: Go beyond a simple IT audit. Evaluate your organizational readiness across multiple dimensions: technical maturity (data infrastructure, legacy dependencies), operational processes (current workflows, manual bottlenecks), and cultural readiness (leadership alignment, workforce skills).
- Perform a Gap Analysis: Identify the specific gaps between your current state and your desired future state. Where are the biggest data silos? Which manual processes are causing the most significant financial drain? This analysis will highlight the areas of greatest need and opportunity.
- Identify and Prioritize Use Cases: Based on your gap analysis, identify a shortlist of potential use cases. Rank them using a matrix that plots potential business impact against implementation complexity. Your initial targets should be in the high-impact, low-complexity quadrant, these are the quick wins that will build momentum and secure broader buy-in for the transformation journey.
2. Planning Phase: Architect the Future
With a clear understanding of your starting point and initial targets, you can now design the architectural and operational plan for your transformation.
- Select Your Technology Stack: Based on your assessment, define the necessary technology stack. This includes decisions on cloud infrastructure (e.g., AWS, Azure, GCP), data integration and API management platforms, and the core AI/ML development and MLOps tools.
- Evaluate Partners and Vendors: This is the critical “build vs. partner” decision point. Analyze whether you have the in-house expertise, resources, and time to build these complex systems from scratch. For most payers, a strategic partnership with an AI specialist who brings proven technology and deep domain expertise is the faster, more reliable, and lower-risk path to value. A thorough evaluation of potential partners’ capabilities, track record, and strategic alignment is paramount here.
- Develop a Phased Timeline and Resource Plan: Create a detailed, realistic roadmap that outlines a phased implementation. Assign clear ownership for each workstream, allocate the necessary budget and personnel, and establish key milestones and KPIs for each phase. This plan becomes the central document for managing the transformation program.
3. Execution Phase: Build, Measure, Learn, Scale
This is where the plan is put into action. The key to success in this phase is an agile, iterative approach and not a rigid, waterfall-style deployment.
- Launch Your First Scalable Pilot: Begin with the top-priority use case identified in the assessment phase. Execute it as a focused, time-bound project with a dedicated cross-functional team. The goal is to get a production-ready solution deployed quickly to demonstrate value.
- Track Success and Broadcast Wins: Meticulously track the KPIs defined in your plan. When you hit a key milestone, for example reducing claims processing time by 50% or identifying your first $1 million in potential fraud, broadcast that success across the organization. These wins are the fuel that powers a long-term transformation journey.
- Create a Feedback Loop for Continuous Optimization: The launch is not the end. Establish a continuous feedback loop where insights from the live system are used to refine and improve the AI models and associated workflows. This “build, measure, learn” cycle, managed through robust MLOps practices, ensures your solutions evolve and deliver increasing value over time.
- Scale and Expand: Use the success and learnings from your initial project to build the business case for the next set of use cases. As you execute more projects and your AI maturity grows, you can begin connecting these capabilities to unlock exponential, cross-functional value across the enterprise.
Partner vs. Build: The Strategic Decision That Defines Your Trajectory
As you stand at the precipice of transformation, you face a fundamental choice: do you commit your own resources to build these complex AI systems from the ground up, or do you leverage a strategic partner who has already paved the way?
This decision will have a greater impact on the speed, cost, and ultimate success of your initiative than almost any other.
The Allure and the Reality of Building In-House
The desire to build a proprietary solution is understandable. It promises complete control, a system perfectly tailored to your unique specifications, and the development of valuable in-house expertise. However, the reality of this path is fraught with hidden complexities and risks that are often underestimated.
- Massive Resource Commitment: Building even a single production-grade data integration can require a team of 6-8 specialists working for over six months. Now, multiply that effort across the dozens of connections and systems required for enterprise AI. The talent required: specialized data engineers, MLOps experts, and AI researchers is scarce and expensive.
- The Time-to-Value Chasm: The development lifecycle for enterprise AI systems is long. From initial architecture to data ingestion, model training, testing, and deployment, an in-house build can take 18-24 months before delivering any significant business value. In the fast-moving healthcare market, this delay can mean ceding critical ground to more agile competitors.
- The Scalability and Maintenance Trap: Building the initial system is only the beginning. The ongoing cost and effort required to maintain, update, and scale these systems are substantial. As new data sources emerge, regulations change, and AI models drift, your internal teams will be locked in a perpetual and costly cycle of maintenance, diverting focus from new innovation.
The Power of Strategic Partnership: Acceleration and De-Risking
A strategic partnership is not simply outsourcing. It is about leveraging specialized expertise and proven technology to accelerate your transformation and mitigate risk. The data shows this is the preferred path for a reason: 61% of executives choose to partner with specialists to drive their digital initiatives.isg-one
- Accelerated Time-to-Value: A partner with a mature platform and pre-built connectors can collapse implementation timelines from years to months. They bring a ready-made solution for the undifferentiated heavy lifting like data ingestion, normalization, security, and infrastructure, allowing you to focus immediately on applying AI to solve your unique business problems.
- Access to Proven, World-Class Expertise: Leading AI partners live and breathe this technology. They have dedicated teams of specialists who have already solved the complex problems you are just beginning to encounter. This instantly infuses your organization with deep domain knowledge and technical expertise that would take years to build organically.
- Reduced Risk and Predictable Costs: A partnership model typically involves more predictable costs and shifts the risk of technological obsolescence from you to the partner. They are responsible for keeping the platform at the cutting edge, ensuring you always have access to the latest capabilities without bearing the full R&D burden.
- Focus on Your Core Business: Your organization’s core competency is healthcare, not building enterprise AI platforms. A strategic partnership allows your team to remain focused on what they do best: managing risk, improving member health, and optimizing provider networks while leveraging a powerful AI engine to do it better.
The right partner acts as an extension of your team. They bring the technology, the talent, and the roadmap to turn your transformation vision into a reality faster, more efficiently, and with a greater certainty of success.
The Transformation Imperative
The healthcare payer industry is at a strategic inflection point. The traditional models that have governed operations for decades are no longer sustainable. With financial pressures mounting and agile, tech-forward competitors entering the market, the question is no longer if payers must transform, but how quickly they can execute.
The $200 billion in value currently locked away in your systems is not just a latent opportunity; it is the fuel required to survive and thrive in the coming decade.
Waiting is no longer a viable strategy. The pace of technological advancement and the urgency of the market demand decisive action. Sticking with the status quo, grappling with legacy systems, underutilized data, and manual processes is a conscious choice to fall behind.
The path to success is not about launching more isolated pilot projects or incrementally improving broken processes. It requires a bold, holistic vision and a commitment to executing a strategic blueprint.
The journey involves building a solid data foundation, targeting high-ROI use cases, and scaling AI capabilities across the enterprise. It demands a culture that embraces data-driven decision-making and a leadership team that has the courage to move beyond familiar but failing paradigms.
The most critical decision on this journey is whether to walk the path alone or with an expert guide. For most, the complexity, cost, and risk of building these systems in-house are prohibitive.
A strategic partnership with an AI specialist de-risks the journey and dramatically accelerates your time-to-value, allowing you to focus on what you do best: running your business.
The blueprint is clear. The technology is ready. The ROI is proven. The time to act is now.