Key Takeaways
• Data silos cost millions annually – Poor data quality drains $12.90 million yearly while eliminating silos can save $4 million in operational efficiencies alone.
• Five pillars form the foundation – Successful payer data strategies require governance, architecture integration, quality management, advanced analytics, and robust security frameworks.
• 97% of healthcare data goes unused – Despite generating 50 petabytes annually, most organizations can’t effectively leverage their information due to fragmented systems and poor integration.
• Technical solutions need organizational buy-in – FHIR standards and APIs enable interoperability, but success depends on change management and stakeholder alignment across departments.
• Assessment drives transformation – Organizations must conduct comprehensive analytics readiness evaluations before implementing roadmaps to bridge current capabilities with future vision.
Healthcare payer data has reached a tipping point. McKinsey analysis shows Enterprise AI solutions could save healthcare payers $150 million to $300 million in administrative costs and $380 million to $970 million in medical costs for every $10 billion of revenue, while simultaneously increasing revenues by $260 million to $1.24 billion [13]. The opportunity is massive.
The reality? Most organizations can’t access the value hidden in their own data.
Healthcare generates 50 petabytes of data annually, yet 97% goes completely unused because it remains unstructured [11]. Staffing pressures compound the problem and estimates point to a deficit of up to 124,000 physicians by 2033 and the need to hire at least 200,000 nurses annually [12]. Healthcare payers acquire data from multiple disconnected systems, creating information silos that undermine analytics efforts [12].
That disconnect is costly.
Despite unprecedented technological capabilities, legacy systems and fragmented operations keep organizations locked in inefficiency [13]. Your data flows like water through leaky, disconnected pipes—abundant in volume but never reaching its destination to generate power.
This blueprint addresses the fundamental challenge: how to rebuild your data infrastructure to capture real value. We’ll examine the current state of healthcare payer data, outline five essential pillars of an effective data strategy, provide a practical implementation roadmap, and offer specific approaches to eliminate the silos blocking true integration.
Every critical decision in your payer operations hinges on data [13]. The foundation needs to be solid.
The Current State of Data in Healthcare Payer Organizations
Most healthcare payer organizations operate with data infrastructure built like an old house: additions stacked over decades, functional but far from optimal. The storm clouds are gathering.
Common data challenges across payer systems
Healthcare payers face 8% year-on-year medical cost trends for the group market in 2025 [1]. That’s just the beginning. Value-based care initiatives demand new capabilities. CMS health equity standards keep evolving. HEDIS ratings require constant attention. Emerging drug therapies need integration into policy plans [1].
Each challenge exposes the same underlying weakness: most payers lack the data infrastructure to respond with speed and precision.
The iceberg problem persists. What you see above the surface is your structured, accessible data, representing less than 50% of structured healthcare data actively used, while only 1% of unstructured data ever gets analyzed [2].
The siloed data problem and its impact
Data silos operate like departmental fortresses. Impressive walls. Poor communication.
Over 60% of healthcare executives identify these silos as major barriers to effective analytics [13]. Nearly 80% of healthcare data remains unstructured and inaccessible [13], locked away from predictive insights that could change outcomes.
One regional health insurer eliminated their silos and saved nearly $4 million annually in operational efficiencies [13]. Without centralized data, clinical personnel can’t make real-time care management decisions, creating risks for members and organizations alike [13].
The cost of fragmentation is measurable. The benefit of integration is proven.
Data quality issues in healthcare payer analytics
Poor data quality creates a foundation of quicksand. Organizations lose approximately $12.90 million annually [1] while data scientists spend 50-80% of their time cleaning and preparing data before analysis begins [1].
Four out of five provider directory entries in the five largest private health plans contain inaccuracies [4]. Physician practices spend $2.76 billion annually maintaining these directories [4].
That’s not a data problem. That’s a business problem.
Gaps in governance and compliance frameworks
70% of healthcare organizations still lack formal data governance strategy [2]. The result? Vulnerability to compliance failures and reputational damage. Healthcare data breaches increased 17.9% month-over-month in April 2025, affecting approximately 10.26 million individuals [5].
Resource constraints amplify the challenge—70% of payer organizations cite these limitations as major obstacles to effective governance [2].
The gaps are real. But so are the solutions. Torsion’s solutions for healthcare helps organizations build robust governance frameworks, while our GenAI Weather Map provides clear assessment of your current readiness.
Five High-Impact Pillars of Healthcare Payer Data Strategy
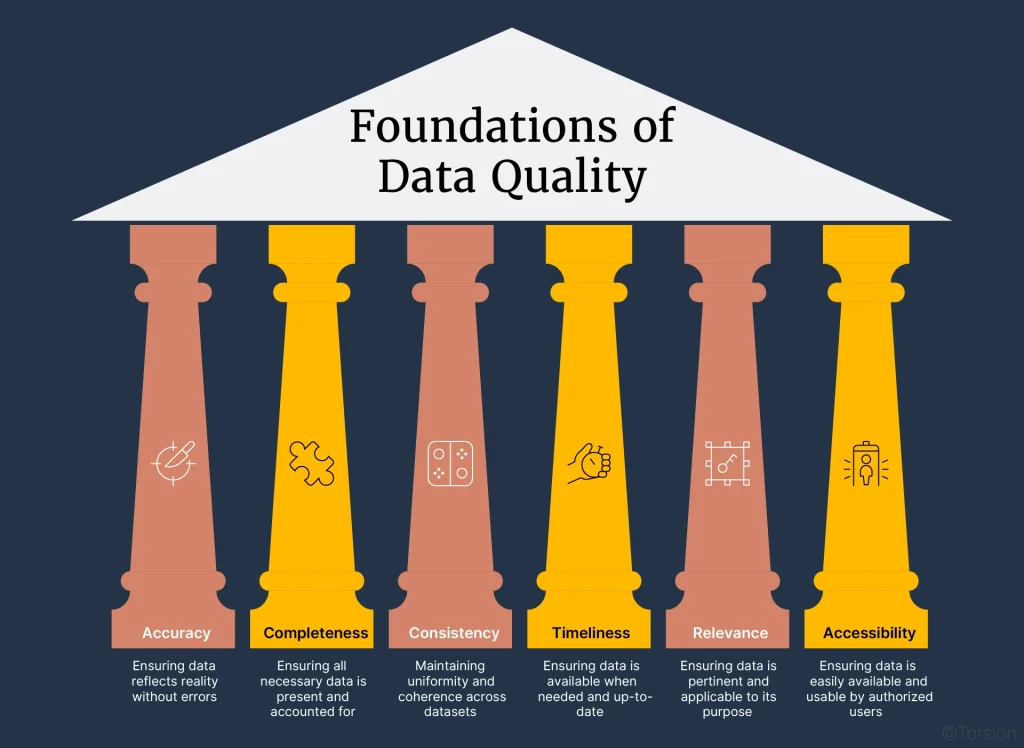
Building an effective healthcare payer data strategy is essential for survival in today’s complex environment. Five critical pillars form the foundation of a robust approach that delivers measurable results.
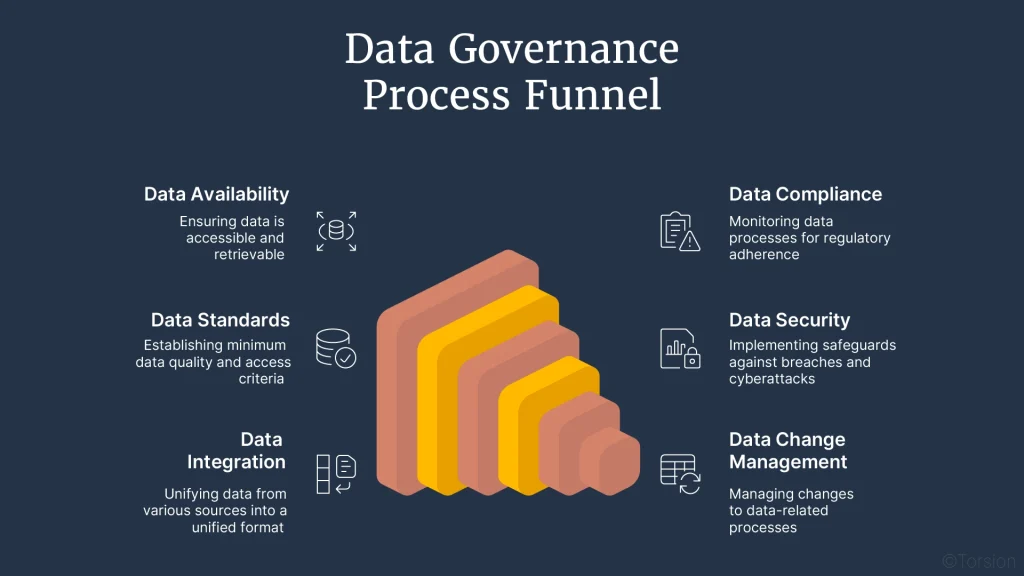
1. Data governance and stewardship
Data governance functions as the operating system for your entire data ecosystem, establishing policies for access, management, and permissible uses while stewardship handles daily implementation. This governance framework ensures data integrity and security through clear policies and standards [6].
Healthcare data stewardship requires managing data assets to ensure accuracy, integrity, and usability across organizations [7]. Effective governance identifies individuals who oversee compliance efforts, manage access controls, and monitor data usage to prevent breaches [8].
2. Data architecture and integration
Solid data architecture operates like the circulatory system of your organization—invisible when functioning properly, catastrophic when it fails. Healthcare payers need architecture that follows a systematic approach, enabling flow from unstructured collections to actionable insights [9].
Most payer organizations struggle with dozens of data silos maintained by business units across different technologies [10]. Developing “data products”, high-quality, ready-to-use data sets for reuse across the organization, breaks down these organizational barriers [10].
3. Data quality management
Poor data quality costs organizations approximately $12.90 million annually [11]. Healthcare payers must prioritize quality through automated validation rules ensuring incoming data adheres to predefined formats and standards [12].
One regional health insurer eliminated data silos and saved nearly $4 million annually in operational efficiencies through improved data quality initiatives. Standardized protocols for data entry reduce variability and inconsistencies [12].
4. Advanced analytics capabilities
Advanced analytics transforms raw data into competitive advantage. Leading payers commit up to 10% of administrative budgets to analytics capabilities [13]. Smart investments focus on solving critical business problems rather than building infrastructure alone [13].
Organizations that excel in analytics hire “integrators”, people whose understanding of business value and analytics helps translate data insights into operational results [13].
5. Security and compliance frameworks
The Security Rule establishes national standards to protect electronic health information, requiring administrative, physical, and technical safeguards [14]. Frameworks like HITRUST CSF help healthcare organizations comply with regulations and protect information [15].
These five pillars work together to create data infrastructure that drives business value, ensures compliance, and positions your organization for sustained competitive advantage.
Ready to assess your position? Download our eBook to evaluate your readiness and learn implementation strategies. Our healthcare industry expertise helps organizations build data foundations that deliver results.
Building Your Healthcare Payer Data Roadmap

Data roadmaps aren’t wishful thinking, they’re strategic blueprints that connect current reality with high-impact outcomes. Your roadmap needs architectural precision before you break ground on transformation.
Assessment and current state analysis
Start with honest evaluation. Comprehensive analytics readiness assessment evaluates three critical components: organizational structure, technology landscape, and staff skills [16]. This assessment positions your organization along the analytics adoption model compared to industry benchmarks [17].
The evaluation examines your ability to support business objectives across five areas: leadership culture, financial alignment, analytics capabilities, best practices, and adoption [17]. Direct exploration of your existing data environment provides the honest starting point required for meaningful progress.
Defining a future-state vision
Position data as a strategic enabler, not just operational support. One large health plan worked with consultants to design a future-state vision that transformed provider data from siloed assets into strategic advantage [18]. Winning visions solve specific business problems rather than build infrastructure for its own sake.
Gap analysis and prioritization
Bridge current state with desired future through systematic gap identification. This process determines what measures need implementation to achieve required compliance levels [19]. Gartner reports that 66% of payer CIOs prioritize investments in consumer experience capabilities, which rely heavily on high-quality data [20].
Implementation planning and execution
Create implementation plans that account for normal operations and other strategic initiatives [21]. Change management requires ongoing communication through regular touchpoints including townhalls, progress updates, and stakeholder alignment sessions [3].
Remember: implementation isn’t a single event but a sustained effort requiring consistent momentum.
Measurement and continuous improvement
Establish metrics that drive decisions throughout execution [3]. Healthcare needs evolve rapidly, so develop data strategies that maintain flexibility over time [22]. Consider partnerships with providers for regular clinical data exchange to enhance your strategic position.
Visit Torsion’s optimization and governance services to learn how our expertise can help establish metrics that measure your data strategy’s effectiveness.
Breaking Down Data Silos: Practical Approaches
Data silos demand dismantling, not discussion. Poor data quality costs organizations $12.90 million annually [1], the barriers aren’t optional anymore.
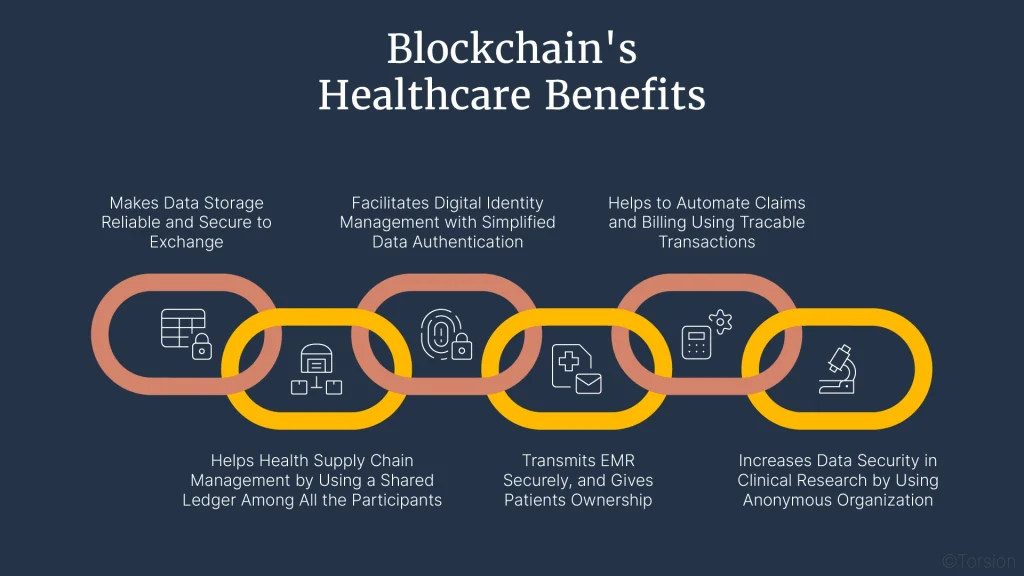
Technical solutions for interoperability
HL7’s Fast Healthcare Interoperability Resources (FHIR) has become the gold standard for healthcare data exchange. FHIR enables disparate systems to communicate through standardized protocols without forcing complete system overhauls [23]. Think of universal translators, not universal languages.
Application Programming Interfaces (APIs) function as digital bridges between systems. APIs allow different software applications to communicate seamlessly, enabling data flow across previously isolated platforms [23]. For healthcare payers specifically, API implementation improves electronic sharing between payer and provider, or between two payers [23].
Centralized data platforms that normalize information across sources deliver measurable results. Upcycling technology improved data usability from 49% to 83% across major clinical domains in one implementation [24].
Organizational alignment and change management
Technical solutions fail without human adoption. Early stakeholder engagement creates the foundation—cast a vision for why change matters and how it benefits everyone involved [25]. Healthcare organizations find success appointing change leaders from different departments to create smoother transitions [25].
Team resistance often stems from unfamiliarity with new systems. Comprehensive training and documentation addressing specific departmental concerns builds confidence and drives adoption [25].
Partner ecosystem strategies for data sharing
The most successful payer organizations create collaborative ecosystems with providers. Referencing the same clinical data and evidence-based information between benefit teams and with providers aligns policy designs internally while smoothing payer-provider relationships [1].
Ready to scale your interoperability solutions enterprise-wide? Learn how Torsion can help or download our GenAI Weather Map to assess your organization’s readiness for next-generation data sharing.
Moving from Data Chaos to Strategic Advantage
Healthcare payer data strategy stands at a critical juncture. This guide has exposed the industry paradox: drowning in 50 petabytes of annual data while utilizing less than 3% effectively. That disconnect costs millions while leaving transformative opportunities on the table.
The five pillars we’ve explored: governance, architecture, quality management, analytics capabilities, and security frameworks, function like structural supports of a bridge. They connect your current operations to future possibilities. Without any one element, the entire structure collapses under increasing data volumes and regulatory demands.
Your path forward starts with an honest assessment. Payers can’t transform without understanding their current data maturity. Breaking down silos becomes less about technical solutions alone and more about creating organizational culture that views data as a shared strategic asset.
This transformation requires both commitment and expertise. Many organizations need specialized guidance to navigate between legacy systems and modern data infrastructure. Contact Torsion to discuss how we can help transform your healthcare payer data strategy: https://torsion.ai/contact-us/
Healthcare continues evolving at unprecedented speed. Value-based care models and consumer expectations drive constant change. Your data strategy represents more than an IT initiative, it’s the cornerstone of competitive advantage and operational excellence.
Organizations that master their data now will outpace those still struggling with fragmented systems. The time to act is immediate.
Data without strategy creates noise. Data with purpose becomes your most powerful asset for delivering better healthcare outcomes at lower costs. This transformation is about fundamentally reimagining how your organization harnesses information to fulfill its mission.
The healthcare ecosystem demands digital excellence. Your data foundation determines whether you lead or lag behind.
References
[1] – https://www.mckinsey.com/industries/healthcare/our-insights/rewiring-healthcare-payers-a-guide-to-digital-and-ai-transformation
[2] – https://healthtechmagazine.net/article/2024/07/data-differentiator-how-integrated-data-strategy-supports-healthcare-ai-success
[3] – https://pmc.ncbi.nlm.nih.gov/articles/PMC12075486/
[4] – https://www.tenasol.com/blog/enterprise-clinical-data-strategy-how-ai-is-leading-the-way
[5] – https://www.inovaare.com/blog/leadership-role-in-data-strategies-for-healthcare-payers/
[6] – https://www.wolterskluwer.com/en/expert-insights/aligning-payer-data-and-teams-critical-to-address-current-challenges
[7] – https://www.linkedin.com/pulse/why-data-governance-non-negotiable-healthcare-payers-david-sullivan-ts82e
[8] – https://www.hashstudioz.com/blog/healthcare-data-silos-challenges/
[9] – https://www.dataideology.com/case-study/eliminating-data-silos-saves-healthcare-payer-nearly-4-mm-yearly/
[10] – https://solutionsreview.com/data-management/why-healthcare-payers-are-leaking-revenue-over-data-quality/
[11] – https://www.metricstream.com/blog/healthcare-risk-compliance-key-challenges.html
[12] – https://www.harmonyhit.com/healthcare-data-stewardship/
[13] – https://www.gaine.com/articles/how-data-stewardship-protects-healthcare-organizations
[14] – https://www.alation.com/blog/building-data-compliance-framework-comprehensive-guide/
[15] – https://www.growthjockey.com/blogs/guide-for-healthcare-payers-on-data-architecture
[16] – https://www.wolterskluwer.com/en/expert-insights/the-cost-benefit-of-data-quality-and-strategy-in-healthcare
[17] – https://www.gaine.com/blog/data-quality-management-in-healthcare-the-complete-guide
[18] – https://www.bcg.com/publications/2018/boosting-health-care-payer-performance-advanced-analytics
[19] – https://www.hhs.gov/hipaa/for-professionals/security/laws-regulations/index.html
[20] – https://www.healthcatalyst.com/learn/insights/5-ways-hitrust-common-security-framework-protects-data
[21] – https://www.healthcatalyst.com/learn/white-papers/healthcare-analytics-for-payers-how-to-thrive-through-shifting-financial-risk
[22] – https://www.healthcatalyst.com/learn/insights/healthcare-analytics-payers-roadmap
[23] – https://www.healthscape.com/insights/prioritizing-alignment-how-health-plan-developed-enterprise-provider-data-strategy
[24] – https://www.hipaajournal.com/gap-analysis-in-healthcare/
[25] – https://insights.vitaldatatechnology.com/healthcare-payer-strategic-priorities-insights-from-gartners-2025-cio-agenda
[26] – https://www.phdata.io/blog/data-strategy-framework-healthcare-providers/
[27] – https://healthedge.com/resources/blog/healthcare-payer-digital-transformation-top-3-strategic-plan-execution-tips
[28] – https://www.wolterskluwer.com/en/expert-insights/a-clear-data-strategy-is-crucial-for-equitable-care
[29] – https://www.symplr.com/blog/healthcare-data-sharing-between-providers-payers
[30] – https://www.availity.com/case-studies/breaking-data-silos-improving-data-quality-for-more-impactful-public-health/
[31] – https://www.aarete.com/insights/change-management-essentials-for-healthcare-payers/